What is osteoarthritis?
Osteoarthritis (OA) is a degenerative joint disease that impacts millions of people in the world. It is the most common type of arthritis and typically affects the knees, hips, hands, and spine. Osteoarthritis can cause pain, stiffness, and swelling in the joints, and can lead to significant disability in severe cases.
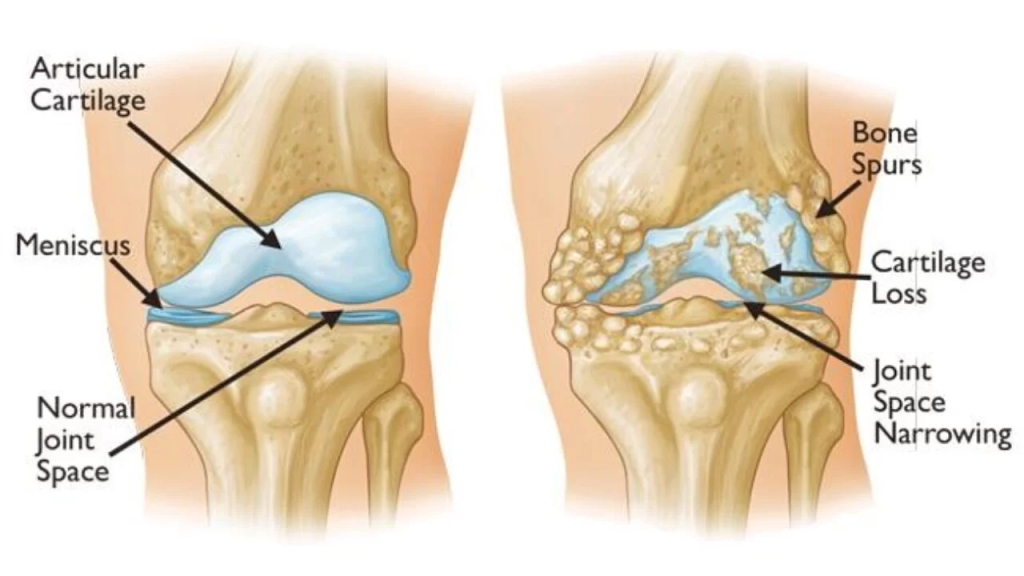
The disease occurs when the cartilage that cushions the joints begins to break down. This can be due to a combination of factors, including age, genetics, joint injury or overuse, and obesity. When cartilage is destroyed, the bones within the joint begin to rub against each other, causing pain and damage to the joint. Osteophytes can develop over time, further limiting the range of motion of the affected joint.
Prevention of osteoarthritis is focused on maintaining a healthy weight, exercising regularly, and avoiding repetitive joint injuries. There is no cure for osteoarthritis, but with appropriate management, many people with the disease can maintain good quality.
Cause of osteoarthritis:
Osteoarthritis is a complex disease with multiple risk factors and underlying causes. While the exact cause of osteoarthritis is not fully understood, several factors are believed to contribute to its development, including:
- Age: One of the most significant risk factors for osteoarthritis is age. As we age, the body’s ability to repair and maintain cartilage in the joints decreases, leading to its breakdown.
- Genetics: Studies have shown that certain genetic factors can increase the risk of developing osteoarthritis. Individuals with a family history of the disease are more likely to develop it themselves.
- Joint injury or overuse: Repeated injuries or overuse of a joint can lead to the development of osteoarthritis. Athletes, for example, are at higher risk of developing the disease due to the constant wear and tear on their joints.
- Obesity: Being overweight or obese puts additional stress on weight-bearing joints, such as the hips and knees. This can accelerate the breakdown of cartilage and increase the risk of developing osteoarthritis.
- Hormonal changes: Changes in hormones, particularly estrogen in women, have been linked to the development of osteoarthritis.
- Other medical conditions: Certain medical conditions, such as diabetes, gout, and rheumatoid arthritis, can increase the risk of developing osteoarthritis.
- Inflammation: Chronic low-level inflammation in the body has been linked to the development and progression of osteoarthritis.
While these factors are believed to contribute to the development of osteoarthritis, the exact mechanisms by which they lead to the disease are not fully understood.
Signs and Symptoms of osteoarthritis:
The signs and symptoms of osteoarthritis can vary from person to person and depend on which joints are affected. Symptoms of osteoarthritis can vary depending on the severity of the disease. However, some common signs and symptoms of osteoarthritis include:
- Pain: Osteoarthritis can cause pain in the affected joints, which can be mild to severe. The pain may be worse after physical activity or prolonged periods of inactivity.
- Stiffness: Joint stiffness is a common symptom of osteoarthritis, especially in the morning or after sitting for a long time. Stiffness usually improves with movement and activity.
- Swelling: Swelling and tenderness around the affected joint(s) may occur. Joints may also feel hot.
- Reduced range of motion: As osteoarthritis progresses, joint movement can become limited, making it difficult to perform everyday activities like walking or climbing stairs.
- Cracking or popping sounds: Some people with osteoarthritis may hear a crunching or popping sound when they move the affected joint(s).
- Bone spurs: Bone spurs may develop in advanced cases of osteoarthritis, leading to further damage to the joint and reducing the range of motion.
- Weakness: As osteoarthritis progresses, the muscles around the affected joint(s) may weaken, making it harder to move the joint.
It is essential to note that not everyone with osteoarthritis will experience all of these symptoms, and some people may experience symptoms not listed here. If you have any concerns about joint pain or stiffness, speak to your doctor, who can diagnose the condition and recommend appropriate treatment.
Diagnosis in osteoarthritis:
The diagnosis of osteoarthritis typically involves a physical exam, medical history, and imaging tests such as X-rays or magnetic resonance imaging (MRI). Blood tests are usually not needed to diagnose osteoarthritis.
Osteoarthritis (OA) is typically diagnosed through a combination of medical history, physical examination, and imaging tests.
Medical history: A doctor will ask about symptoms such as joint pain, stiffness, and reduced range of motion, as well as any family history of OA or other joint disorders.
Physical examination: The doctor will examine the affected joint(s), checking for tenderness, swelling, warmth, and range of motion. They may also look for signs of joint deformity or muscle weakness.
Imaging plays an important role in the diagnosis and management of osteoarthritis (OA). Here are some of the imaging techniques used for the diagnosis of OA:
- X-ray: X-rays are typically the first imaging test used to diagnose OA. They can show changes in the joint, such as narrowed joint space, bone spurs, and changes in the shape of the bone, the degeneration of the cartilage in the affected joint. X-rays can also help identify the severity of OA.
- Magnetic resonance imaging (MRI) and computed tomography (CT) scans can also be used to provide more detailed images of the joint and surrounding structures.
- Computed tomography (CT): A CT scan can provide detailed images of the bones and joints, and can be helpful in identifying small fractures and bone deformities. It may be used when an MRI is not possible or when a more detailed image of the bone is required.
- Ultrasound: Ultrasound can be used to diagnose joint damage and inflammation, and it can also help guide injections into the affected joint.
- Imaging tests are an important tool for the diagnosis and management of osteoarthritis.
Laboratory tests: Blood tests are not usually necessary to diagnose OA, but they can help rule out other conditions that may cause similar symptoms, such as rheumatoid arthritis or gout
However, a diagnosis of OA is not based on imaging tests alone, and a combination of clinical assessment and imaging is necessary for an accurate diagnosis.
Ultimately, the diagnosis of OA is based on a combination of these factors, and may also involve ruling out other conditions that can cause joint pain and stiffness. If you suspect you have OA, it’s important to see a doctor for an accurate diagnosis and to discuss treatment options.
Treatment:
Treatment for osteoarthritis aims to relieve symptoms, slow the progression of the disease, and improve joint function.Common treatments include:
- Medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or acetaminophen to relieve pain and reduce inflammation.
- Physical therapy to improve joint mobility, strength, and flexibility.
- Assistive devices such as braces or shoe inserts to reduce stress on the affected joint(s).
- Weight loss, if needed, to reduce stress on weight-bearing joints.
- In severe cases, surgery may be necessary to replace or repair the affected joint(s)
Osteoarthritis (OA) is a degenerative joint disease that affects the cartilage, bone, and other tissues in and around the joints. The goal of treatment is to relieve pain, reduce inflammation, and improve joint function. Treatment options for OA can be divided into medical and surgical interventions.
Medical Treatment:
- Pain relief: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, naproxen, and aspirin, can relieve pain and reduce inflammation.
- Topical medications: Topical NSAIDs, such as diclofenac gel, can be applied directly to the affected joint to provide localized pain relief.
- Injections: Corticosteroid injections can be administered directly into the joint to reduce inflammation and relieve pain.
Physical therapy:
Physical therapy can help strengthen the muscles around the affected joint, improve flexibility and range of motion, and reduce pain.
Weight loss: Losing weight can reduce the stress on weight-bearing joints and improve joint function.
Assistive devices: Assistive devices such as canes, crutches, and knee braces can reduce stress on the affected joint and improve joint function.
Surgical Treatment:
Arthroscopic surgery: Arthroscopic surgery involves the use of a small camera and surgical instruments to remove damaged tissue and bone spurs from the joint.
Joint replacement surgery: Joint replacement surgery interests extracting the damaged joint and replacing it with an artificial joint.
Osteotomy: Osteotomy involves cutting and reshaping the bones around the affected joint to improve alignment and reduce stress on the joint.
Joint fusion: Joint fusion involves permanently joining two bones together to reduce pain and improve joint stability.
The choice of treatment depends on the severity of the OA, the area of the affected joint, and the patient’s overall health.
It is important to consult a healthcare professional to determine the most appropriate treatment option for each case.
Physiotherapy treatment in detail in osteoarthritis:
Physiotherapy is an important component of the management of osteoarthritis (OA). It aims to improve the mobility and function of the affected joint, reduce pain, and prevent further deterioration of the joint. Here are some of the physiotherapy treatments used in the management of OA:
- Exercise therapy: Exercise therapy can help strengthen the muscles around the affected joint, improve flexibility and range of motion, and reduce pain. Specific exercises will depend on the location of the affected joint and the severity of the OA. Examples of exercises include stretching, aerobic exercise, and resistance training.
Here are some exercises that may be helpful for osteoarthritis patients:
Range of motion exercises: These exercises help to improve joint flexibility and reduce stiffness. Examples include shoulder circles, ankle pumps, and wrist rotations.
Range of motion exercises in OA:
Range of motion exercises can be helpful for individuals with osteoarthritis (OA) to maintain joint mobility and flexibility, reduce pain, and improve overall joint function. Here are some examples of range of motion exercises that can be beneficial for OA:
- Shoulder circles: Stand up straight and slowly rotate your shoulders in a circular motion, first in a forward direction and then in a backward direction. Repeat this movement 10-15 times.
- Knee bends: Stand up straight with your feet shoulder-width apart. Slowly bend your knees, keeping your back straight, until you feel a stretch in your quadriceps. Hold the stretch for a few seconds and then slowly straighten your legs. Repeat this movement 10-15 times.
- Hip rotations: Lie on the back with the knees bent and feet flat on the floor. Slowly rotate the hips to one side, keeping the shoulders flat on the ground. Hold the stretch for a few seconds and then rotate the hips to the other side. Repeat this movement 10-15 times.
- Wrist circles: Sit in a chair with your arms resting on a table or armrest. Make a circle with your wrists, moving them clockwise and then counterclockwise. Repeat this movement 10-15 times.
- Ankle rolls: Sit in a chair with feet flat on the ground. Slowly roll the ankles in a circular motion, first in a clockwise direction and then in a counterclockwise direction. Repeat this movement 10-15 times. Remember to always consult with a healthcare provider before starting any new exercise program, especially if a person has any health conditions or concerns.
Isometric exercise in OA:
Isometric exercises can be a useful tool for individuals with osteoarthritis (OA) to improve joint stability, reduce pain, and improve overall joint function. Isometric exercises involve contracting a muscle without moving the joint, which can be beneficial for individuals who may have limited mobility or pain with movement. Here are some examples of isometric exercises that can be beneficial for OA:
- Wall sit: Stand with your back against a wall and slowly lower your body until your knees are bent at a 90-degree angle. Hold this position for 10-30 seconds, then slowly stand back up. Repeat this movement 5-10 times.
- Glute squeeze: Sit in a chair with your feet flat on the floor. Tighten your glute muscles and hold for 10-30 seconds, then release. Repeat this movement 5-10 times.
- Static quadriceps contraction: Sit in a chair with the feet flat on the floor. Straighten one leg and hold it in the air for 10-30 seconds, then lower it back down. Repeat this exercise 5-10 times on each leg.
- Calf raises hold: Stand with your feet shoulder-width apart and slowly rise onto the toes, then hold for 10-30 seconds. Slowly lower back down. Repeat this movement 5-10 times.
- Shoulder blade squeeze: Sit in a chair with your arms at your sides. Squeeze your shoulder blades together and hold for 10-30 seconds, then release. Repeat this movement 5-10 times.
Isometric exercises should be done in a comfortable and pain-free range of motion, and it’s important to start with shorter holds and gradually increase the duration as your strength improves.
Strengthening exercises: These exercises help to improve muscle strength around the affected joint, which can help to reduce pain and improve joint stability. Examples include leg presses, calf raises, and bicep curls.
Strengthening exercises can help individuals with osteoarthritis (OA) improve joint stability, reduce pain, and improve overall joint function. Here are some examples of strengthening exercises that can be beneficial for OA:
- Squats: Stand with your feet shoulder-width apart and slowly lower your body as if you are sitting down in a chair. Keep the back straight and the knees aligned with the toes. Hold the position for a few seconds and then stand back up. Repeat this exercise 10-15 times.
- Step-ups: Step onto a platform or sturdy box with one foot and then step back down. Repeat with the other foot. Make sure to keep the knees aligned with the toes and the back straight. Repeat this step-up exercise 10-15 times on each side.
- Wall push-ups: Stand facing a wall with your arms extended at shoulder height and palms flat against the wall. Slowly bend the elbows and lower the chest toward the wall, then push back up. Repeat this exercise 10-15 times.
- Leg raises: Lie on the back with the knees bent and feet flat on the floor. Tighten the abdominal muscles and lift one leg off the ground, keeping it straight. Hold the position for a few seconds and then lower the leg back down. Repeat the exercise with the other leg. Repeat this exercise 10-15 times on each side of the leg.
- Bicep curls: Hold a light weight in each hand and stand with your feet shoulder-width apart. Bend the elbows and bring the weights up toward the shoulders, then slowly lower them back down. Repeat this exercise 10-15 times.
Remember to always consult with a healthcare provider before starting any new exercise program, especially if you have any health conditions or concerns. It’s also important to start with light weights or resistance and gradually increase as your strength improves.
Aerobic exercises: These exercises help to improve cardiovascular health, maintain a healthy weight, and reduce joint pain. Examples include walking, cycling, and swimming.
Aerobic exercise in OA:
Aerobic exercise can be very beneficial for people with osteoarthritis (OA) as it helps to improve cardiovascular health, reduce inflammation, and increase mobility. Here are some examples of aerobic exercises that are safe and effective for people with OA:
- Walking: Walking is a low-impact exercise that is comfortable on the joints and can be done almost anywhere. Start with short walks and slowly increase the duration and intensity over time.
- Cycling: Cycling is another low-impact exercise that is comfortable on the joints. It can be done on a stationary bike or outdoors. Start with short rides and slowly increase the duration and intensity over time.
- Swimming: Swimming is a great way to get aerobic exercise without putting stress on the joints. Water also provides resistance, which helps to build strength. Try swimming laps or participating in water aerobics classes.
- Dancing: Dancing is a fun and social way to get aerobic exercise. It can be done alone or with a partner. Choose dance styles that are low-impact, such as ballroom dancing or line dancing.
- Elliptical training: Elliptical machines provide a low-impact, full-body workout. Start with short sessions and gradually increase the duration and intensity over time.
It is important to talk to the healthcare provider before starting any new exercise program, especially if person have severe OA or other medical conditions. Start slowly and gradually increase the duration and intensity of the aerobic exercise sessions over time. If you experience pain or discomfort during exercise, stop immediately and consult your healthcare provider.
Stretching exercises: These exercises help to improve flexibility and reduce muscle tension around the affected joint. Examples include hamstring stretches, quad stretches, and hip flexor stretches.
Stretching exercises:
Osteoarthritis (OA) is a common condition that affects the joints, especially in older adults. Stretching exercises can help manage OA by improving joint flexibility, reducing stiffness, and increasing the range of motion. Here are some stretching exercises that can be beneficial for people with OA:
- Quadriceps stretch: Stand near a wall or chair for support. Grab the ankle and pull the heel towards the buttock. Hold the stretch position for 15 to 30 seconds and repeat on the other leg.
- Hamstring stretch: Sit on the edge of a chair with your feet flat on the floor. Slowly straighten one leg and reach towards the toes, keeping the back straight. Hold for 15 to 30 seconds and repeat on the other leg
- Calf stretch: Stand facing a wall with the hands on the wall. Step back with one foot and press the heel down towards the floor. Hold for 15 to 30 seconds and repeat on the other leg.
- Shoulder stretch: Stand with the feet shoulder-width apart and reach one arm across the chest. Use the other arm to pull your elbow towards the chest. Hold for 15 to 30 seconds and repeat on the other arm.
- Neck stretch: Sit in a chair with the feet flat on the floor. Tilt your head to one side and use the hand to gently pull the head further. Hold for 15 to 30 seconds and repeat on the other side.
Remember to start slowly and gradually increase the duration and intensity of the stretching exercises. If a person is experience pain during any of these exercises, stop immediately and consult the healthcare provider.
- Manual therapy: Manual therapy involves hands-on techniques to improve joint mobility and reduce pain. Examples of manual therapy techniques used in OA include joint mobilization and manipulation.
- Modalities: Modalities such as heat, cold, ultrasound, and electrical stimulation can help reduce pain and inflammation in the affected joint.
- Patient education: Patient education involves providing information on OA, its causes, and how to manage it. This may include advice on lifestyle modifications such as weight loss, joint protection strategies, and the use of assistive devices.
- Assistive devices: Assistive devices such as canes, crutches, and knee braces can reduce stress on the affected joint and improve joint function.
- Hydrotherapy: Hydrotherapy involves exercising in a pool of warm water. The buoyancy of the water reduces stress on the affected joint, making it easier to exercise.
- Taping: Taping involves applying adhesive tape to the skin around the affected joint to provide support and reduce pain.
The choice of physiotherapy treatment will depend on the severity of the OA, the location of the affected joint, and the patient’s overall health
A physiotherapist will design an individualized treatment plan based on the patient’s specific needs and goals. It is important to consult a healthcare professional to determine the most appropriate physiotherapy treatment for each individual case.
It is important to work with a physiotherapist to develop a personalized exercise program that takes into account your specific needs and limitations. They can also help to monitor your progress and make adjustments as needed.
Summary:
Osteoarthritis (OA) is a degenerative joint disease that is common among older adults, but can also occur in younger people. It occurs when the cartilage that cushions the joints begins to break down, leading to pain, stiffness, and decreased mobility. OA can affect any joint in the body, but is most commonly seen in the hands, knees, hips, and spine. There is no cure for OA, but it can be managed through a combination of lifestyle modifications, such as weight loss and exercise, and medications, such as pain relievers and anti-inflammatory drugs. In severe cases, surgery may be necessary. It’s important to talk to your healthcare provider if you suspect that you have OA or are experiencing joint pain or stiffness. Early diagnosis and treatment can help to slow the progression of the disease and improve quality of life.
Frequently Asked Questions
What is osteoarthritis?
Osteoarthritis is a degenerative joint disease that results in the breakdown of the protective cartilage that cushions the ends of bones in a joint. This guides to pain, stiffness, and limited mobility.
How is osteoarthritis diagnosed?
Osteoarthritis is typically diagnosed through a combination of physical examination, medical history, and imaging tests such as X-rays or MRI scans.
Can osteoarthritis be prevented?
While osteoarthritis cannot be completely prevented, there are steps you can take to reduce your risk, such as maintaining a healthy weight, staying physically active, avoiding repetitive stress on the joints, and protecting your joints from injury.
What are the treatment options for osteoarthritis?
Treatment options for osteoarthritis include physiotherapy, pain management, lifestyle modifications such as weight loss and exercise, and in severe cases, surgery.
Is osteoarthritis hereditary?
While there is a genetic component to osteoarthritis, it is not entirely hereditary. Other factors, such as lifestyle and environmental factors, can also contribute to the development of osteoarthritis.
Leave a comment